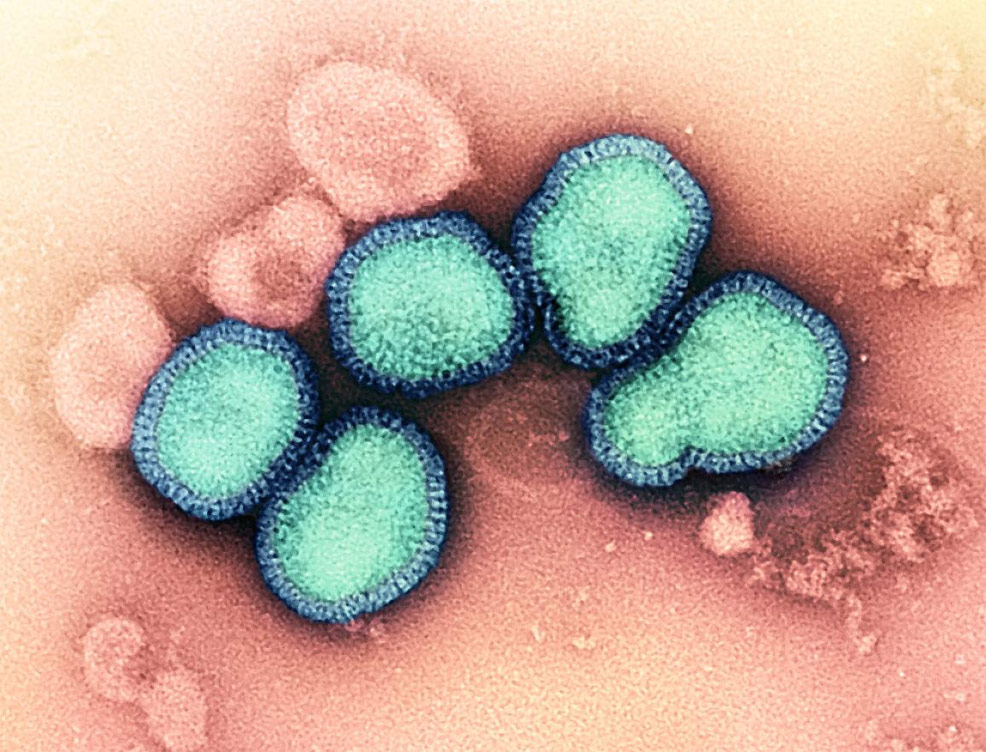
31st May 2023 Universal flu vaccine begins human trials The National Institutes of Health (NIH) has begun a Phase 1 trial of an mRNA-based universal influenza vaccine, enrolling 50 volunteers.
A clinical trial of a universal influenza (flu) vaccine developed by researchers at the National Institutes of Health (NIH) has begun at Duke University in Durham, North Carolina. This Phase 1 trial will test the mRNA-based vaccine – known as H1ssF-3928 mRNA-LNP – for safety and its ability to induce an immune response. mRNA-based therapies represent a paradigm shift in medicine, due to their ability to "instruct" our own cells to produce therapeutic proteins, offering a versatile and efficient means of treatment. Unlike traditional drugs, they can be designed quickly to target various diseases, including those for which there are currently no effective treatments. The future potential of mRNA technology is vast – spanning from rapid vaccine development (as seen with COVID-19), to treating rare genetic diseases, cancer, and more. This trial will enrol up to 50 healthy volunteers aged 18 through 49. Three groups of study participants (10 participants each) will be vaccinated with 10, 25 and 50 micrograms of the experimental vaccine, respectively. After evaluation of the data, another 10 people will be enrolled to receive the optimum dose. The study will also include a group of participants receiving a current quadrivalent seasonal flu vaccine. This will allow the researchers a point of direct comparison between the immunogenicity and safety of the candidate vaccine and available seasonal flu vaccines. Participants will be regularly evaluated to assess the vaccine's safety (and, secondarily, its efficacy) and will receive follow-up appointments within a year of vaccination. Seasonal flu viruses kill thousands of people in the United States each year. The Centers for Disease Control and Prevention estimates that from 2010–2020, between 12,000 and 52,000 people died of flu across the country each year. Although seasonal flu shots are valuable tools in controlling the spread and severity, they do not provide immunity against every strain. Each year, before the flu season begins, scientific experts must predict which strains are likely to be most common during the upcoming months and then select three or four of these strains to include in the next seasonal flu vaccine. Vaccine manufacturers then need time to produce and distribute the vaccine – during which the dominant strains of the virus can change in unexpected ways, potentially decreasing the efficacy of the vaccine. A so-called "universal" flu vaccine could eliminate these problems, by protecting its recipients against a wide variety of strains and ideally providing durable long-term immunity, so people would not need to be vaccinated every year. "A universal influenza vaccine would be a major public health achievement and could eliminate the need for both annual development of seasonal influenza vaccines, as well as the need for patients to get a flu shot each year," said Hugh Auchincloss, MD, Acting Director of the National Institute of Allergy and Infectious Diseases (NIAID), which is part of the NIH. "Moreover, some strains of influenza virus have significant pandemic potential. A universal flu vaccine could serve as an important line of defence against the spread of a future flu pandemic." This early-stage trial is being conducted through the Collaborative Influenza Vaccine Innovation Centers (CIVICs) program, created by the NIAID in 2019 to support the development of broadly protective and longer-lasting flu vaccines. It is the first investigational universal flu vaccine candidate to be assessed by the CIVICs program, and is being manufactured at the Duke Human Vaccine Institute, which is part of Duke University. A similar vaccine developed by researchers at the NIAID's Vaccine Research Center (VRC) has already shown positive results in early trials. Both vaccines use a specific portion of flu protein, hemagglutinin (HA), to induce a broad immune response. While one portion of the HA protein, known as the head, tends to change as the flu virus spreads and evolves, a more stable portion, known as the stem, evolves very slowly and is very similar across many different strains of flu virus. By using the HA stem as the basis for a vaccine, researchers hope to induce long-term immunity against a broad range of flu viruses. Unlike the VRC's earlier vaccine, the new H1ssF-3928 mRNA-LNP vaccine candidate uses a messenger RNA (mRNA) platform. By developing and testing a variety of different platforms for a universal flu vaccine, researchers are more likely to find one that is both safe and effective.
Comments »
If you enjoyed this article, please consider sharing it:
|