27th October 2023 Breakthrough in treatment of cervical cancer A breakthrough in treating cervical cancer is reported, with participants in a recent trial achieving a five-year survival rate of 80% – up from the previous average of 70%. The study used a combination of existing, cheap drugs ahead of usual radiotherapy treatment.
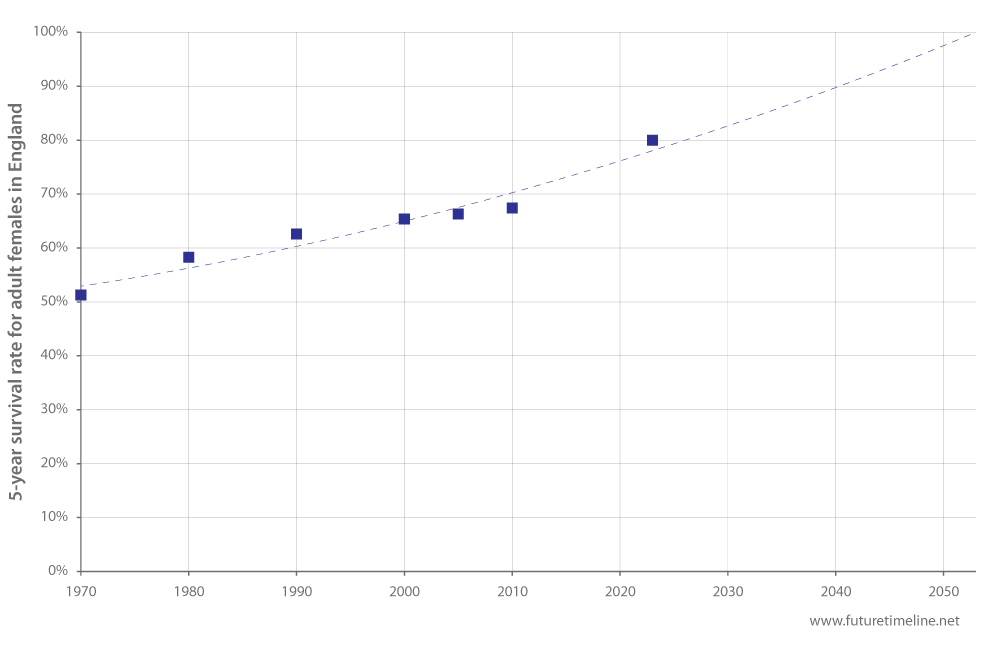
Phase III of the INTERLACE trial, funded by Cancer Research UK and University College London (UCL) Cancer Trials Centre, assessed whether a short course of induction chemotherapy (IC) prior to chemoradiation (CRT) could reduce the rate of relapse and death among patients with cervical cancer. Researchers involved in the study presented the preliminary results at the recent European Society for Medical Oncology (ESMO) congress. Each year, around 3,200 new cases of cervical cancer are diagnosed in the UK. Peak incidence occurs in women during their early thirties. CRT has been the standard treatment for cervical cancer since 1999, but despite improvements in radiation therapy techniques, the cancer returns in up to 30% of cases. For the INTERLACE trial, 500 patients with a median age of 46 took part in hospitals over the course of 10 years. Each had been diagnosed with cervical cancer large enough to be seen without a microscope, but which had not yet spread to other parts of the body. Patients were randomly allocated to receive either standard CRT (external radiation with weekly cisplatin and brachytherapy), or an initial six-week course of IC (carboplatin and paclitaxel chemotherapy) followed by the same standard CRT described above. After five years, 80% of those who received IC plus CRT were alive and 73% had not seen their cancer return or spread. In the standard treatment group, 72% were alive and 64% had not seen their cancer return or spread. "This is the biggest improvement in outcome in this disease in over 20 years," said Dr Mary McCormack, lead investigator of the trial from UCL Cancer Institute and UCLH. "I'm incredibly proud of all the patients who participated in the trial; their contribution has allowed us to gather the evidence needed to improve treatment of cervical cancer patients everywhere. We couldn't have done this without the generous support of Cancer Research UK." In recent decades, the five-year survival rate for cervical cancer in England appeared to be reaching a plateau of around 65-70% (according to the government's latest available data). This new breakthrough is a major boost to the long-term historical trend, which could potentially lead to 100% survival by mid-century.
Because the drugs required for IC – carboplatin and paclitaxel – are cheap, accessible, and already approved for use in patients, the study authors say they could be incorporated into standard of care treatment relatively quickly. "Cervical cancer is a disease that often strikes women in their thirties or younger," said Professor Jonathan Ledermann, senior author of the results from UCL Cancer Institute. "Those with locally advanced disease have a relatively high chance of relapse and the disease can take a huge toll on patients and their families. This makes the results of the INTERLACE trial, which significantly improves overall survival, an important advance in treatment." Dr Iain Foulkes, Executive Director of Research and Innovation at Cancer Research UK, said: "Timing is everything when you're treating cancer. The simple act of adding induction chemotherapy to the start of chemoradiation treatment for cervical cancer has delivered remarkable results in this trial. A growing body of evidence is showing the value of additional rounds of chemotherapy before other treatments like surgery and radiotherapy in several other cancers. Not only can it reduce the chances of cancer coming back, it can be delivered quickly using drugs already available worldwide."
Comments »
If you enjoyed this article, please consider sharing it:
|