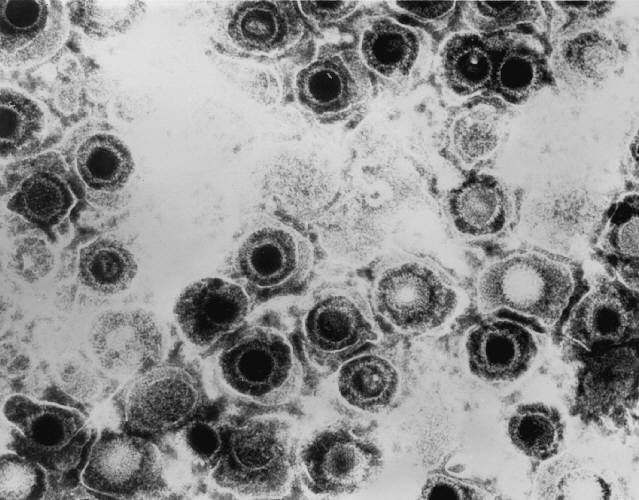
11th May 2013 Another step closer to a herpes vaccine Researchers have achieved a significant breakthrough in understanding genital herpes, which could lead to the development of a vaccine to prevent and treat HSV-2.
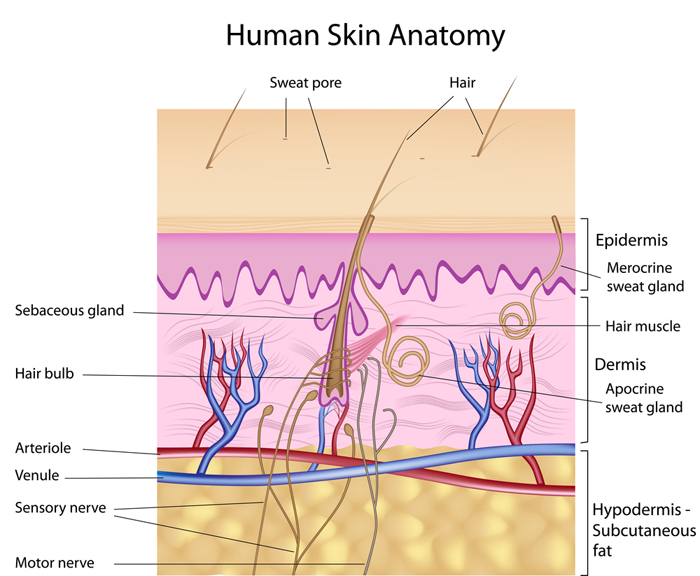
Scientists have identified a class of immune cells that reside long-term in the genital skin and mucosa, and are believed to be responsible for suppressing recurring outbreaks of genital herpes. These immune cells also play a role in suppressing symptoms of genital herpes, which is why most sufferers of the disease are asymptomatic when viral reactivations occur. The discovery of this subtype of immune cells, called CD8αα+ T cells, opens a new avenue of research to develop a vaccine to prevent and treat herpes simplex virus type 2, or HSV-2. Identifying these T cells’ specific molecular targets, called epitopes, is the next step in developing a vaccine. Larry Corey, M.D., an internationally renowned virologist who is president of the Fred Hutchinson Cancer Research Center: “The discovery of this special class of cells that sit right at the nerve endings where HSV-2 is released into skin is changing how we think about HSV-2 and possible vaccines. For the first time, we know the type of immune cells that the body uses to prevent outbreaks. We also know these cells are quite effective in containing most reactivations of HSV-2. If we can boost the effectiveness of these immune cells, we are likely to be able to contain this infection at the point of attack and stop the virus from spreading in the first place. We’re excited about our discoveries because these cells might also prevent other types of viral infections, including HIV infection.” According to the Centers for Disease Control and Prevention, more than 776,000 people in the US are newly infected with herpes annually. Nationwide, 16.2 percent, or about one out of six people aged 14 to 49, have genital HSV-2. There is currently no effective vaccine. “While antiviral treatment is available, the virus often breaks through this barrier and patients still can transmit the infection to others,” Corey said. “In addition, newborn herpes is one of the leading infections transmitted from mothers to children at the time of delivery. An effective genital herpes vaccine is needed to eliminate this complication.” Jia Zhu, co-author of the study, which appears in Nature: “The cells we found perform immune surveillance and contain the virus in the key battlefield where infection occurs, which is the dermal-epidermal junction. These cells are persistent in the skin and represent a newly discovered phenotype distinguished from those of CD8+ T cells circulating in the blood.”
“We did not expect to find CD8αα+ T cells in the skin,” Zhu said. “This was a surprise.”
Comments »
|