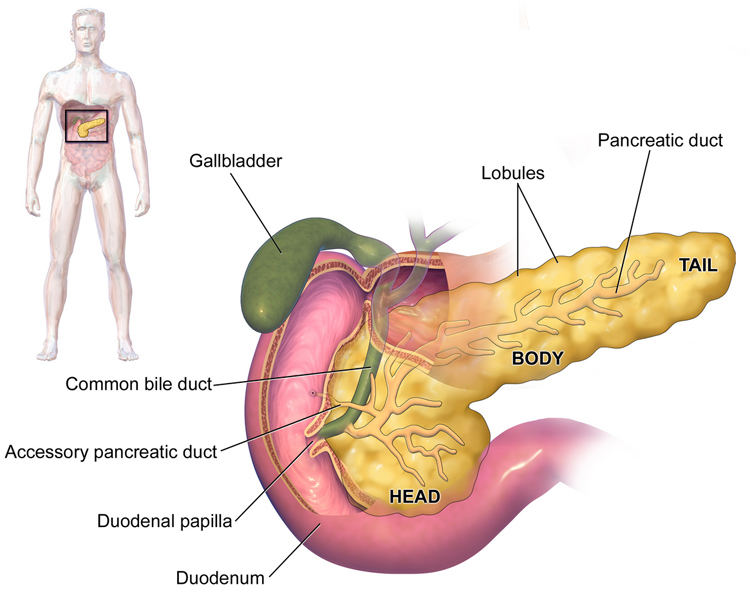
27th June 2015 Two important breakthroughs in pancreatic cancer Pancreatic cancer is among the deadliest known cancers, with a very low survival rate. Two separate but related studies were recently published that offer new hope for both detecting and treating the disease.
In the USA, the five-year survival rate for pancreatic cancer is only around 7 per cent. Progress towards finding a cure has been very slow compared to other types of cancer with only small, incremental advances over the last few decades. At the current rate of progress, it will take almost two centuries for the survival figure to reach 100 per cent (see "When will cancer be cured?"). As death rates from other cancers begin to fall, the Pancreatic Cancer Action Network predicts that pancreatic cancer will rise from the 4th to the 2nd leading cause of cancer death by 2020. Part of what makes pancreatic cancer so deadly is the fact that it tends to be detected at a very late stage. By the time a patient knows they have it, options for treatment are very limited and in many cases it is already terminal. Improving the early detection and diagnosis of the illness to expose hidden tumours has been a major focus of research. This week, a new study by the M.D. Anderson Cancer Centre, part of the University of Texas, was published in the journal Nature. The paper describes a protein that is found on exosomes (tiny particles released by cancer cells). This protein results in "cancer exomes" that are known as GPC1+ crExos. Researchers were able to distinguish – with 100% accuracy – between healthier patients with a benign pancreatitic disease, and those with early stage pancreatic cancer itself – based on the presence of this protein. Levels of the protein were much lower after surgical removal of tumours. This finding could lead to a blood test that would allow doctors to screen for pancreatic cancer much more effectively. "GPC1+ crExos were detected in small amounts of serum from about 250 patients with pancreatic cancer with absolute specificity and sensitivity, importantly distinguishing patients with [non-cancerous] pancreatitis from those with early- and late-stage pancreatic cancer," says Dr. Raghu Kalluri, chair of Cancer Biology, in an accompanying press release. "This presents an unprecedented opportunity for informative early detection of pancreatic cancer and in designing potential curative surgical options." In addition, he says: "GPC1+ crExos can be detected and isolated in blood samples that were stored in freezers almost 30 years ago, unlike circulating tumour cells (CTCs) that require large amounts of fresh blood. DNA, RNA and proteins can be isolated from cancer exosomes isolated from stored specimens for further genetic and biological analyses. Therefore, cancer exosomes are not just a biomarker – but isolating them provides a trove of cancer-specific information." The study found that GPC1+ crExos detected the possibility of pancreatic cancer in mouse models, at a time when the mice showed no signs of pancreatic disease from MRI scans. "Routine screening of the general population for pancreatic cancer using MRIs or CTs would be prohibitively expensive with the likelihood for many false positives," says David Piwnica-Worms, Ph.D., chair of Cancer Systems Imaging. "Our study suggests the potential for GPC1+ crExos as a detection and monitoring tool for pancreatic cancer in combination with imaging – with an emphasis on its application in early detection."
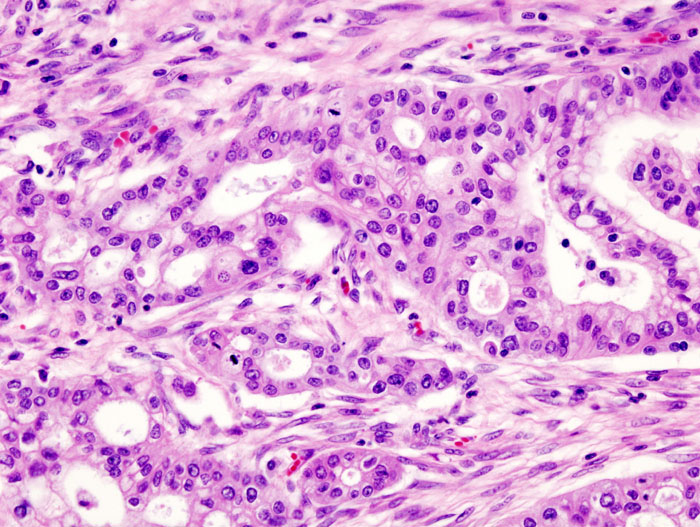
A second, separate paper was published this month in the journal Scientific Reports. This study explains how scientists from University College London (UCL) designed a new chemical compound, able to reduce the growth of pancreatic cancer tumours in mice by 80%. This compound – known as MM41 – can block faulty genes by targeting little knots in their DNA, called quadruplexes, which are very different from normal DNA and are especially found in faulty genes. It is confirmed that MM41 has a strong inhibiting effect on two genes – k-RAS and BCL-2 – both of which are found in the majority of pancreatic cancers. The UCL team, led by Professor Stephen Neidle, conducted a small-scale trial involving two groups of eight mice with pancreatic tumours using different doses of the compound, twice a week for 40 days. A further control group received no treatment. The tumours in the group given the larger dose decreased by an average of 80% during the treatment period, and after 30 days, regrowth stopped in all the mice. For two of the mice in this group, the tumour disappeared completely with no signs of regrowth at all following the end of treatment, for a further 239 days (equivalent to the rest of their average natural life span). Analysis of the mice tumours showed that the MM41 compound had been taken up into the nucleus of the cancer cells, showing that it was able to effectively target the pancreatic cancer tumour. No significant side effects were observed on the mice during the study: there was no damage to other tissue or organs and none of the mice showed any significant weight loss. Discussing the results, Neidle explained: "This research provides a potentially very powerful alternative approach to the way that conventional drugs tackle pancreatic cancer, by targeting a very specific area of the DNA of faulty genes. One of the genes that MM41 blocks – the BCL-2 gene – is involved in regulating apoptosis, the body's natural process which forces cells to die if they become too damaged or unhealthy to be repaired. BCL-2 is present in high amounts in many tumours and helps cancer cells to survive, but when the BCL-2 gene is blocked by MM41 in mice, the cancer cells succumb to apoptosis and die." Neidle stresses that although these results are exciting, MM41 is not ideal for trialling in humans and further refinements are needed: "We are now working to optimise this class of compounds, but it's clearly worthy of further investigation for potential use in treating pancreatic cancer in people."
Comments »
|