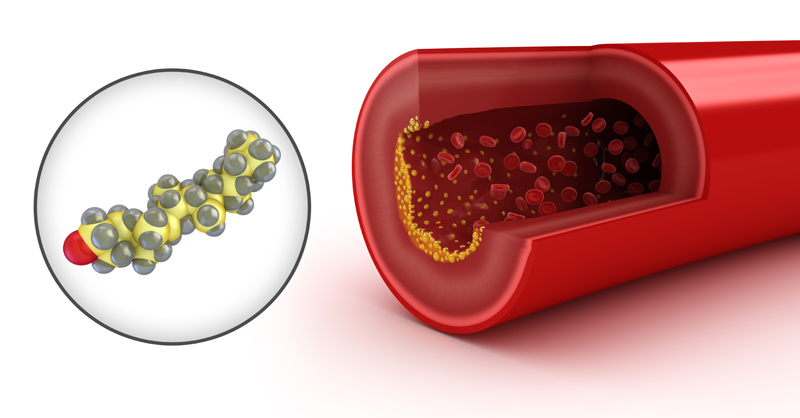
7th May 2019 Researchers identify key process linked to plaque formation in blood vessels Researchers at UT Southwestern Medical Center have determined how circulating "bad cholesterol" enters artery walls, causing the plaque that narrows the blood vessels and leads to heart attacks and strokes. Since low-density lipoprotein, or LDL, cholesterol entry into the artery wall drives the development of atherosclerosis, or hardening of the arteries, which in turn leads to heart attacks and strokes, future treatments blocking the process may help decrease the occurrence of these life-threatening conditions. Cardiovascular disease is the no. 1 cause of death worldwide, and coronary artery disease (which underlies heart attacks) and strokes account for over 60% of cardiovascular deaths in the U.S., according to statistics from the American Heart Association (AHA). The new study, published in Nature, reveals for the first time how a protein called SR-B1 (short for "scavenger receptor class B, type 1") ferries LDL particles into and then across the endothelial cells that line arteries. The study also found that a second protein, called dedicator of cytokinesis 4, or DOCK4, partners with SR-B1 for the process.
In the early stages of atherosclerosis, LDL that has entered the artery wall attracts and is engulfed by important immune system cells called macrophages that ingest, or "eat," LDL particles. These LDL-laden macrophages become "foam cells" that promote inflammation and further the development of plaques. The plaques narrow the artery and can become unstable. Plaques that rupture can activate blood clotting and block blood flow to the brain or heart, resulting in a stroke or heart attack. In studies of mice with elevated cholesterol, the scientists determined that deleting SR-B1 from the endothelial cells lining blood vessels resulted in far less LDL entering the artery wall, fewer foam cells formed, and plaques that were considerably smaller. "At the start of this work, it was surprisingly unknown how LDL enters the artery wall to cause cardiovascular disease," said Dr. Philip Shaul, Director of the Center for Pulmonary and Vascular Biology at UT Southwestern. "The paper's findings solve that mystery – and counter many scientists' prior assumption that LDL simply enters through sites of damage or disruption in the single layer of endothelial cells that serves as the artery wall's protective barrier." In their studies, the researchers compared SR-B1 and DOCK4 abundance in areas of the mouse aorta that are prone to plaque formation, with regions less likely to become atherosclerotic. They found higher levels of SR-B1 and DOCK4 in the disease-prone regions long before plaques formed, which suggests that atherosclerotic lesions may be more common in particular artery sites because of more SR-B1 and DOCK4 present there. To determine if these findings might apply to people, the team reviewed data on atherosclerotic and normal arteries from humans in three independent databases maintained by the National Institutes of Health (NIH). In all three databases, SR-B1 and DOCK4 were more abundant in atherosclerotic arteries compared with normal arteries. The researchers are now exploring the possibility of gene therapy to switch off or reduce the function of SR-B1 and DOCK4 proteins in the endothelial cells that line arteries, in order to prevent atherosclerosis, Dr. Shaul said. "If you could develop a drug that inhibits SR-B1 or DOCK4 – or a gene therapy that silences them in endothelial cells – you could potentially decrease atherosclerosis and, hence, reduce the incidence of coronary artery disease, heart attack, and stroke," he said. "Such strategies would complement current treatments that lower circulating LDL and be particularly valuable in situations in which LDL lowering is challenging."
Comments »
If you enjoyed this article, please consider sharing it:
|