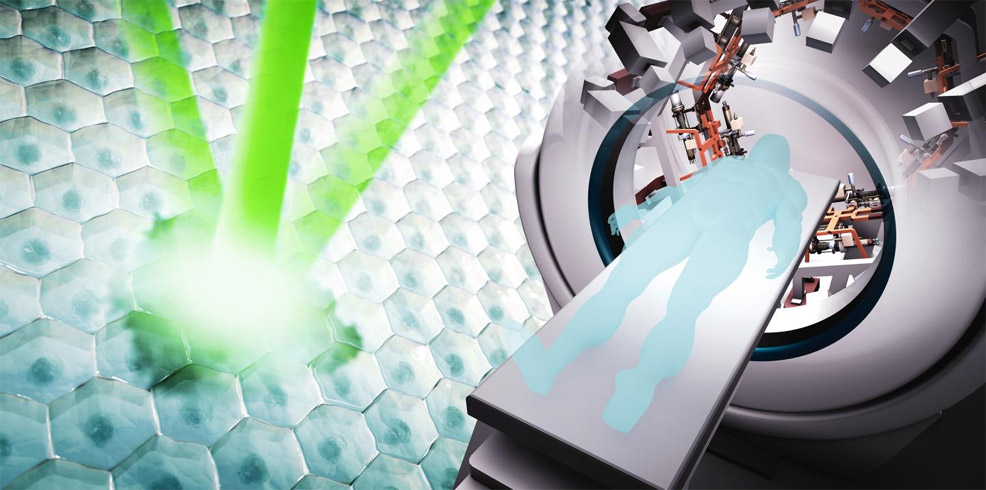
3rd December 2018 Future devices for cancer treatment could zap tumours in less than a second New machines, which could see human clinical trials in the 2020s, will reduce the side effects of radiation therapy by vastly shrinking the length of a typical session.
New accelerator-based technology being developed by the U.S. Department of Energy's SLAC National Accelerator Laboratory and Stanford University aims to reduce the side effects of cancer radiation therapy, by shrinking its duration from minutes to under a second. Built into future compact medical devices, technology developed for high-energy physics could also help make radiation therapy more accessible around the world. The SLAC/Stanford team has now received crucial funding to proceed with two projects – one using X-rays, the other using protons. The idea behind both is to blast cancer cells so quickly that organs and other tissues don't have time to move during the exposure, like taking a single freeze frame from a video. This can reduce the chance that radiation will hit and damage neighbouring healthy tissue around tumours, making radiation therapy more precise. "Delivering the radiation dose of an entire therapy session with a single flash lasting less than a second would be the ultimate way of managing the constant motion of organs and tissues, and a major advance compared with methods we're using today," said Billy Loo, an associate professor of radiation oncology at Stanford School of Medicine. "In order to deliver high-intensity radiation efficiently enough, we need accelerator structures that are hundreds of times more powerful than today's technology. The funding we received will help us build these structures," said Sami Tantawi, a professor of particle physics and astrophysics from SLAC. The first project, called PHASER, will develop a flash delivery system for X-rays. In today's medical devices, electrons fly through a tube-like accelerator structure that's about a metre long, gaining energy from a radiofrequency field that travels through the tube at the same time and in the same direction. The energy of the electrons then gets converted into X-rays. Over the past few years, the PHASER team has developed and tested accelerator prototypes with special shapes and new ways of feeding radiofrequency fields into the tube. These components are already performing as predicted by simulations and are paving the way for accelerator designs that support more power in a compact size. "Next, we'll build the accelerator structure and test the risks of the technology, which, in three to five years, could lead to a first actual device that can eventually be used in clinical trials," said Tantawi.
The second project is based on a proton beam, rather than X-rays. In principle, protons are less harmful to healthy tissue than X-rays because they deposit their tumour-killing energy in a more confined volume inside the body. However, proton therapy requires large facilities to accelerate protons and adjust their energy. It also uses magnets weighing hundreds of tons that slowly move around a patient's body to guide the beam into the target. "We want to come up with innovative ways to manipulate the proton beam that will make future devices simpler, more compact and much faster," said Emilio Nanni, a staff scientist at SLAC, who leads the project with Loo and Tantawi. That goal could soon be within reach, thanks to a $1.7 million grant from the DOE Office of Science Accelerator Stewardship program to develop the technology over the next three years. "We can now move forward with designing, fabricating and testing an accelerator structure similar to the one in the PHASER project that will be capable of steering the proton beam, tuning its energy and delivering high radiation doses practically instantaneously," Nanni said. Another key objective for both projects is to make radiation therapy more accessible. Today, millions of patients worldwide can receive only palliative care, because they lack access to cancer therapy. The team is designing systems that are compact, power-efficient, economical, efficient to use in clinical settings and compatible with existing infrastructure in countries around the world. "We hope that our work will contribute to making the best possible treatment available to more patients in more places," said Loo.
Comments »
If you enjoyed this article, please consider sharing it:
|